Diagnosing AADC
deficiency
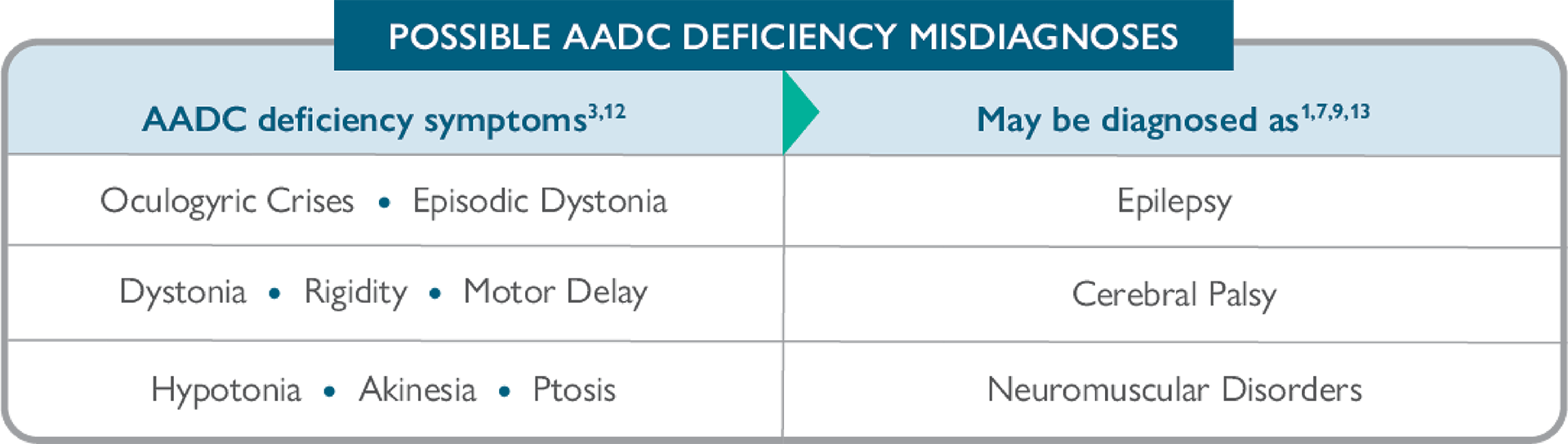
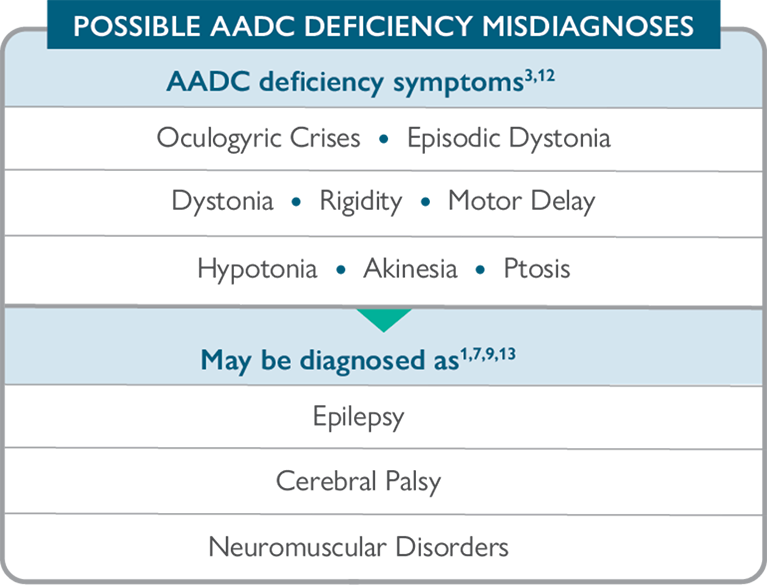
AADC deficiency may be misdiagnosed or go undiagnosed, delaying treatment and proper management 3,4,12
Despite symptom onset during infancy, diagnosis is typically delayed 3:
Symptoms of neurotransmitter disorders can overlap with those of other neurological disorders, which can make diagnosis challenging. Many of the most common symptoms of AADC deficiency can also be attributed to a number of other conditions such as cerebral palsy and epilepsy, resulting in potential misdiagnosis.1-4,7-9
The challenge of a correct diagnosis:
conditions with symptoms similar to those of AADC deficiency
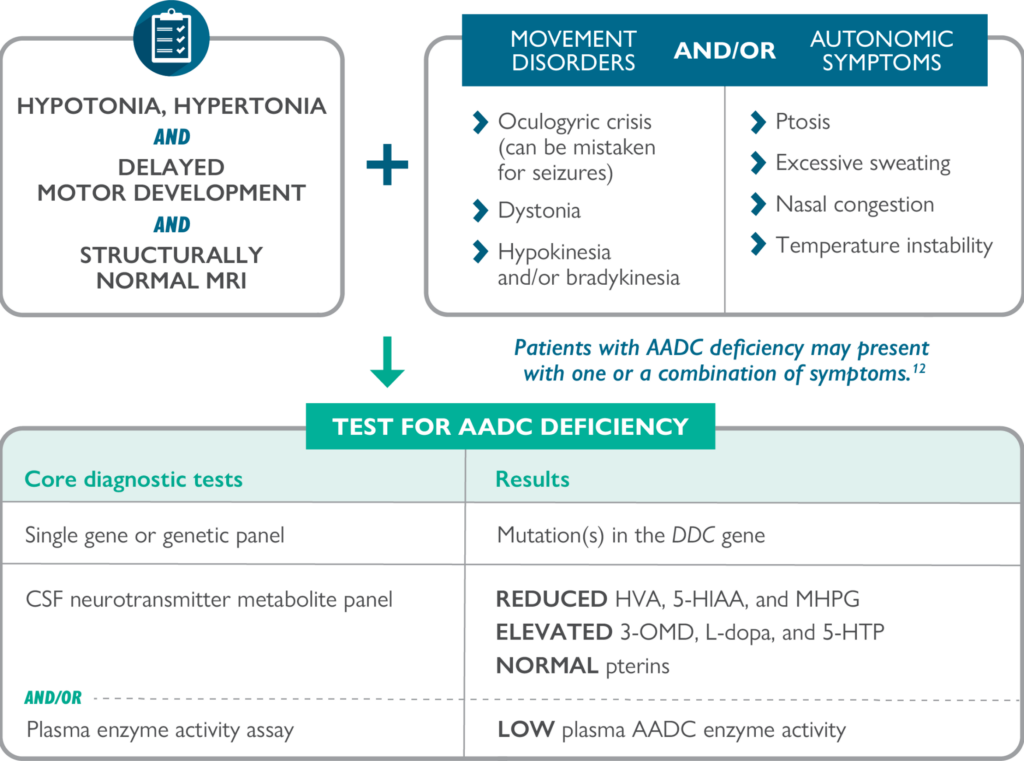
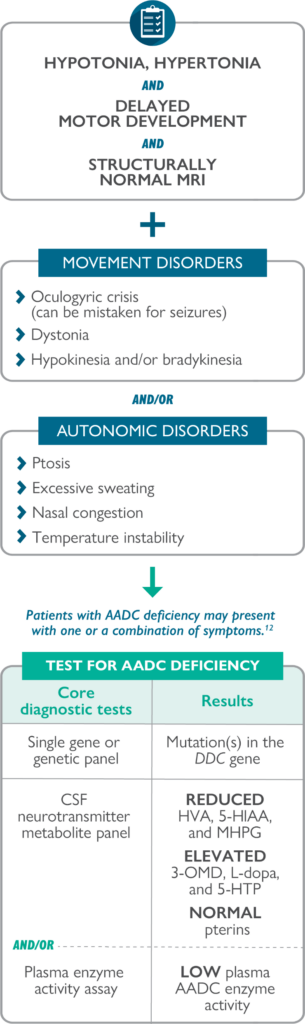
Look for key differentiating signs and symptoms of AADC deficiency
One or a combination of the following red-flag diagnostic clues should prompt investigation for a neurotransmitter disorder, including AADC deficiency:
CT=computer tomography; EEG=electroencephalogram; MRI=magnetic resonance imaging.

Accurate identification can help improve the care and management of patients with AADC deficiency10,12
Diagnostic pathway for suspected AADC deficiency 3,12
Other tests that may be helpful include16-19:
Blood level measurement of 3-OMD
Urinary organic acid analysis


Download a Diagnosis Guide to help confirm AADC deficiency
Why test for 3-OMD?
Reduced AADC enzyme activity causes an increase in L-dopa, 3-OMD, and 5-HTP, and a decrease in the neurotransmitter metabolites HVA and 5-HIAA.3,4,10,11
References
1. Ng J, Papandreou A, Heales SJ, et al. Monoamine neurotransmitter disorders—clinical advances and future perspectives. Nat Rev Neurol. 2015;11(10):567-584. 2. Ng J, Heales SJR, Kurian MA. Clinical features and pharmacotherapy of childhood monoamine neurotransmitter disorders. Pediatr Drugs. 2014;16(4):275-291. doi: 10.1007/s40272-014-0079-z. 3. Wassenberg T, Molero-Luis M, Jeltsch K, et al. Consensus guideline for the diagnosis and treatment of aromatic l-amino acid decarboxylase (AADC) deficiency. Orphanet J Rare Dis. 2017;12(1):12. doi: 10.1186/s13023-016-0522-z. 4. Brun L, Ngu LH, Keng WT, et al. Clinical and biochemical features of aromatic L-amino acid decarboxylase deficiency. Neurology. 2010;75(1):64-71. 5. Manegold C, Hoffmann GF, Degen I, et al. Aromatic L-amino acid decarboxylase deficiency: clinical features, drug therapy and follow-up. J Inherit Metab Dis. 2009;32(3):371-380. 6. Hwu W-L, Chien Y-H, Lee N-C, et al. Natural history of aromatic L-amino acid decarboxylase deficiency in Taiwan. JIMD Rep. 2018;40:1-6. doi: 10.1007/8904_2017_54. 7. Kurian MA, Dale RC. Movement disorders presenting in childhood. Continuum (Minneap Minn). 2016;22(4):1158-1185. 8. Zouvelou V, Yubero D, Apostolakopoulou L, et al. The genetic etiology in cerebral palsy mimics: the results from a Greek tertiary care center. Eur J Paediatr Neurol. 2019;23(3):427-437. doi: 10.1016/j.ejpn.2019.02.001. 9. Krigger KW. Cerebral palsy: an overview. Am Fam Physician. 2006;73(1):91-100. 10. Pons R, Ford B, Chiriboga CA, et al. Aromatic L-amino acid decarboxylase deficiency: clinical features, treatment, and prognosis. Neurology. 2004;62(7):1058-1065. 11. Hwu W-L, Lee N-C, Chien Y-H, et al. AADC deficiency: occurring in humans, modeled in rodents. Adv Pharmacol. 2013;68:273-284. 12. Himmelreich N, Montioli R, Bertoldi M, et al. Aromatic amino acid decarboxylase deficiency: molecular and metabolic basis and therapeutic outlook. Mol Genet Metab. 2019;127(1):12-22. doi: 10.1016/j.ymgme.2019.03.009. 13. Lee W-T. Disorders of monoamine metabolism: inherited disorders frequently misdiagnosed as epilepsy. Epilepsy Seizure. 2010;3(1):147-153. doi: 10.3805/eands.3.147. 14. Pearson TS, Gilbert L, Opladen T, et al. AADC deficiency from infancy to adulthood: symptoms and developmental outcome in an international cohort of 63 patients. J Inherit Metab Dis. 2020;43(5):1121-1130. doi: 10.1002/jimd.12247. 15. Pearson TS, Pons R, Ghaoui R, et al. Genetic mimics of cerebral palsy. Mov Disord. 2019;34(5):625-636. 16. Monteleone B, Hyland K. Case report: discovery of 2 gene variants for aromatic L-amino acid decarboxylase deficiency in 2 African American siblings. BMC Neurol. 2020;20(1):12. doi: 10.1186/s12883-019-1596-8. 17. Chen P-W, Lee N-C, Chien Y-H, et al. Diagnosis of aromatic L-amino acid decarboxylase deficiency by measuring 3-Omethyldopa concentrations in dried blood spots. Clin Chim Acta. 2014;431:19-22. 18. Chien Y-H, Chen P-W, Lee, N-C, et al. 3-O-methyldopa levels in newborns: result of newborn screening for aromatic L-amino-acid decarboxylase deficiency. Mol Genet Metab. 2016;118(4):259-263. doi: 10.1016/j.ymgme.2016.05.011. 19. Brennenstuhl H, Kohlmüller D, Gramer G, et al. High throughput newborn screening for aromatic L-amino-acid decarboxylase deficiency by analysis of concentrations of 3-O-methyldopa from dried blood spots. J Inherit Metab Dis. 2020;43(3):602-610. doi: 10.1002/jimd.12208.