Understanding and
diagnosing AADC
deficiency
Recognising signs and symptoms of AADC deficiency
Neurotransmitter disorders are increasingly recognised as an expanding group of inherited neurometabolic syndromes that affect children
Within a growing group of genetic conditions referred to broadly as neurotransmitter disorders, many are marked by a disruption in monoamine neurotransmitter synthesis, metabolism, and homeostasis.
Neurotransmitter deficiency can lead to a range of neurological manifestations in childhood, including1,2:
Developmental delay
Motor disorders
Epilepsy
Autonomic dysfunction
Neuropsychiatric features
One neurotransmitter disorder is Aromatic L-amino Acid Decarboxylase (AADC) deficiency, which is a genetic disorder associated with defects in neurotransmitter synthesis that can lead to a manifestation of a broad spectrum of symptoms.
Many of the most common symptoms of AADC deficiency can also be attributed to a number of other conditions such as cerebral palsy and epilepsy, resulting in potential misdiagnosis.1-4,7-9
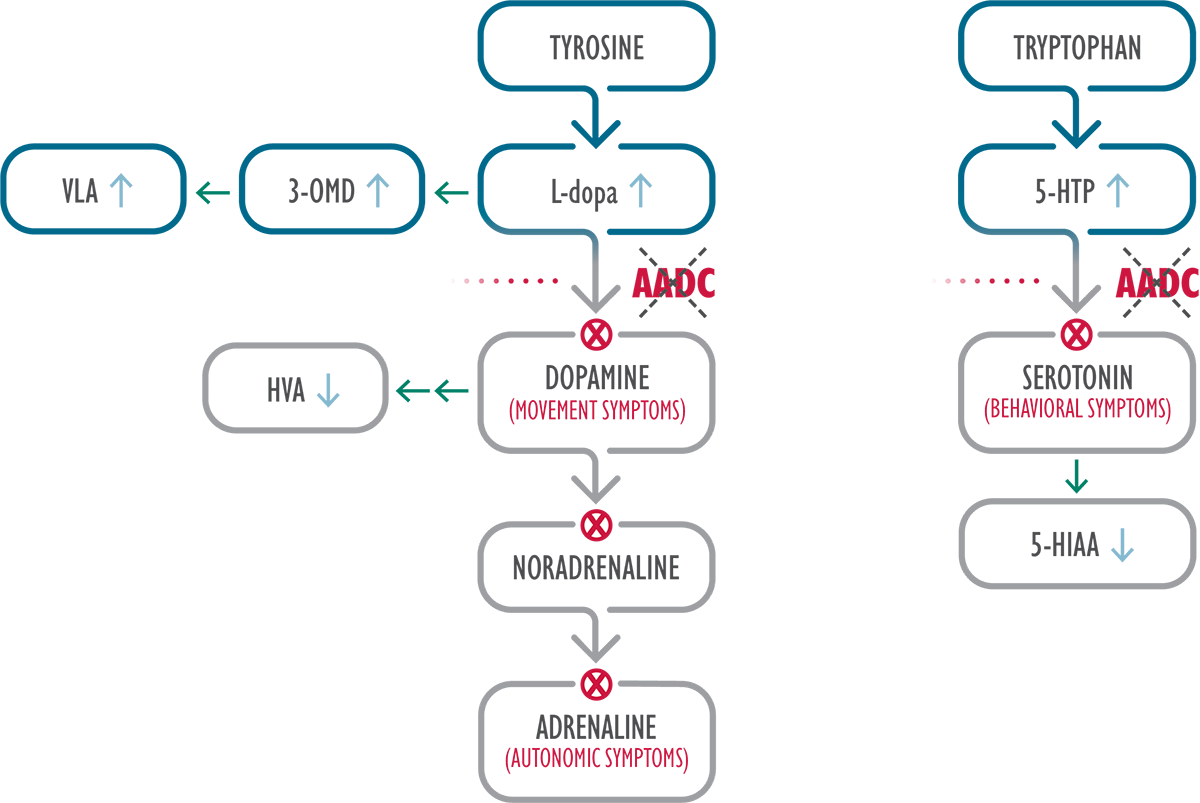
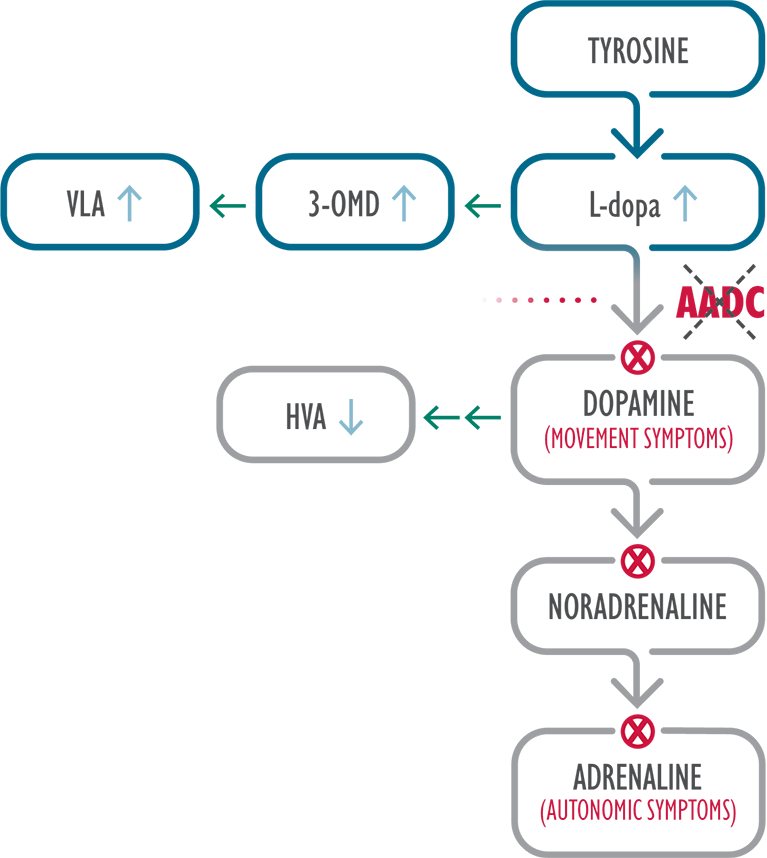
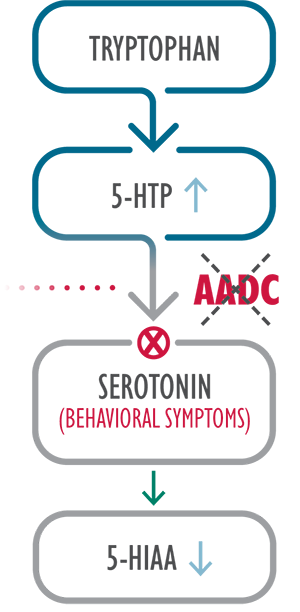
AADC is an enzyme required for biosynthesis of dopamine and serotonin 3
In AADC deficiency, mutations in the dopa decarboxylase (DDC) gene result in reduced AADC enzyme activity, leading to severe combined deficiency of the neurotransmitters dopamine, serotonin, noradrenaline and adrenaline.3,4,10,11
3-OMD=3-O-methyldopa; 5-HIAA=5-hydroxyindoleacetic acid; 5-HTP=5-hydroxytryptophan; HVA=homovanillic acid; L-dopa=L-3,4-dihydroxyphenylalanine; VLA=vanillactic acid.

Recognise the signs and symptoms of AADC deficiency
In a clinical study of 78 patients who were diagnosed with AADC deficiency, the following symptoms were documented 4:

Hypotonia 4
Most commonly reported symptom

Developmental delay 4
In AADC deficiency, developmental delay may include impairments in
head control, crawling, or standing, and speech delays3,6

Movement disorders
Oculogyric crises 4
Episodes of sustained upward or lateral deviation of the eyes, rhythmic orofacial movements, backward and lateral flexions of the neck, tongue protrusion, and jaw spasms11
Can last a few seconds or persist for several hours, and occur several times per day or week10
May not be present in all cases4
Often misdiagnosed as a seizure, epilepsy, or mitochondrial disease10,13

Patients may present with other movement
disorders or symptoms, including 4:
Dystonia (53%) n=41
Hypertonia (44%) n=35
Hypokinesia (32%) n=25
Autonomic symptoms include 4:
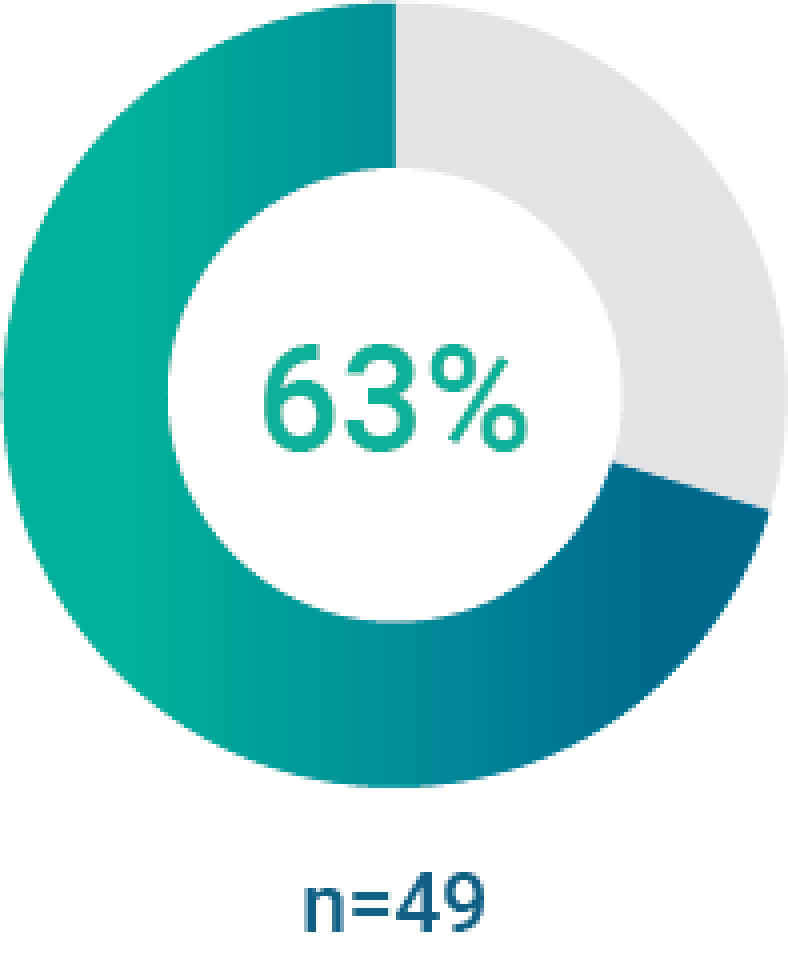
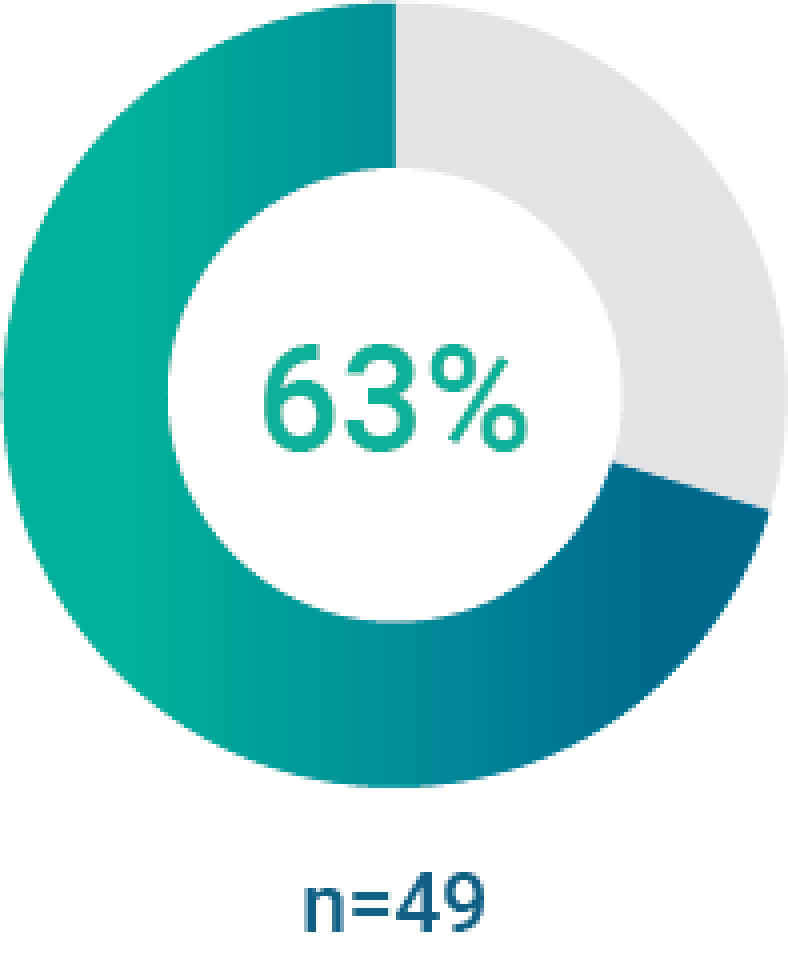
Hyperhidrosis (65%) n=51
Hypersalivation (41%) n=32
Ptosis (39%) n=30
Nasal congestion (31%) n=24

Learn more about the symptoms that should
prompt an investigation of AADC deficiency
References
1. Ng J, Papandreou A, Heales SJ, et al. Monoamine neurotransmitter disorders—clinical advances and future perspectives. Nat Rev Neurol. 2015;11(10):567-584. 2. Ng J, Heales SJR, Kurian MA. Clinical features and pharmacotherapy of childhood monoamine neurotransmitter disorders. Pediatr Drugs. 2014;16(4):275-291. doi: 10.1007/s40272-014-0079-z. 3. Wassenberg T, Molero-Luis M, Jeltsch K, et al. Consensus guideline for the diagnosis and treatment of aromatic l-amino acid decarboxylase (AADC) deficiency. Orphanet J Rare Dis. 2017;12(1):12. doi: 10.1186/s13023-016-0522-z. 4. Brun L, Ngu LH, Keng WT, et al. Clinical and biochemical features of aromatic L-amino acid decarboxylase deficiency. Neurology. 2010;75(1):64-71. 5. Manegold C, Hoffmann GF, Degen I, et al. Aromatic L-amino acid decarboxylase deficiency: clinical features, drug therapy and follow-up. J Inherit Metab Dis. 2009;32(3):371-380. 6. Hwu W-L, Chien Y-H, Lee N-C, et al. Natural history of aromatic L-amino acid decarboxylase deficiency in Taiwan. JIMD Rep. 2018;40:1-6. doi: 10.1007/8904_2017_54. 7. Kurian MA, Dale RC. Movement disorders presenting in childhood. Continuum (Minneap Minn). 2016;22(4):1158-1185. 8. Zouvelou V, Yubero D, Apostolakopoulou L, et al. The genetic etiology in cerebral palsy mimics: the results from a Greek tertiary care center. Eur J Paediatr Neurol. 2019;23(3):427-437. doi: 10.1016/j.ejpn.2019.02.001. 9. Krigger KW. Cerebral palsy: an overview. Am Fam Physician. 2006;73(1):91-100. 10. Pons R, Ford B, Chiriboga CA, et al. Aromatic L-amino acid decarboxylase deficiency: clinical features, treatment, and prognosis. Neurology. 2004;62(7):1058-1065. 11. Hwu W-L, Lee N-C, Chien Y-H, et al. AADC deficiency: occurring in humans, modeled in rodents. Adv Pharmacol. 2013;68:273-284. 12. Himmelreich N, Montioli R, Bertoldi M, et al. Aromatic amino acid decarboxylase deficiency: molecular and metabolic basis and therapeutic outlook. Mol Genet Metab. 2019;127(1):12-22. doi: 10.1016/j.ymgme.2019.03.009. 13. Lee W-T. Disorders of monoamine metabolism: inherited disorders frequently misdiagnosed as epilepsy. Epilepsy Seizure. 2010;3(1):147-153. doi: 10.3805/eands.3.147